Texan's Guide to Cobra Coverage and Alternatives
Cobra is always a confusing mess to people either losing or leaving their jobs and employer coverage.
We're going to walk through all the practical questions we get daily from people all over Texas but more importantly we'll address the question we get daily...
"Help! Is there a cheaper option than Cobra?"
There can be a bit of sticker shock with your Cobra offer letter so we'll cover that as well.
First, our credentials:
This is what we'll cover as our top questions that come our way on Cobra:
- What is Cobra in Texas?
- How long do I have to say yes to Cobra?
- When does Cobra start?
- Can I piecemeal Cobra coverage?
- How long does Cobra last for?
- Can I lose Cobra coverage otherwise?
- How does Cobra compare to exchange plans (ACA, Obamacare, etc)
- How does Cobra compare to short term health plans?
Of course, you can reach out with any questions.
There's zero cost for our assistance:
Call 800-320-6269
help@texasplans.com
Chat online here
Pick a time to talk here
Let's get started!
What is Cobra in Texas?
Cobra is a continuation of your prior employer plan with you paying the full premium now.
Exact same coverage as before but treated like a personal plan. If you had dependents enrolled, they will also have the option to enroll and in fact, Cobra eligibility can be a qualifying event to change plans and/or who is enrolled.
Check with your employer HR department or carrier directly.
Generally, employer coverage goes through the end of the month in which you were terminated unless the termination day was the 1st. In that case, the plan may end right then on the 1st!
You should receive a Cobra offer letter which requires you to "opt in" for the coverage. This means, you won't get Cobra unless you say yes and submit payment!
How long do I have to say yes to Cobra?
Generally, it's 60 days from the last day of employer coverage. You'll receive a letter which states the exact date by which you need to opt-in to get the coverage.
For example, if you left a job on May 15th, the employer plan usually covers you through the end of May. You would have June and July to opt-in to Cobra.
When does Cobra start?
If you opt-in for Cobra and pay the first month's premium, the effective date will go back retroactive to the last day of employer coverage.
For example, if you opt-in for Cobra mid-July, the effective date will be June 1st in the above situation.
You must pay back premiums for both June and July, which can be a big bill!
Can I piecemeal Cobra coverage?
Generally, yes! You can carve up who to cover between family members and coverages.
For example, you may want coverage just for yourself or only for dental and vision but not medical.
Check your Cobra offer for rates and options. We've seen families split between Cobra and Texas Exchange plans based on needs.
How long does Cobra last for?
The standard duration of Cobra is 18 months.
During this period, you can move to the Texas Exchange plans during open enrollment (November 1st - January 15th) or through a special enrollment trigger.
Can I lose Cobra coverage otherwise?
Cobra only exists if the underlying employer plan still exists. If the company closes or cancels the plan, Cobra coverage ends as well.
Also, missing a payment will result in cancellation, and it's extremely difficult (basically impossible) to reinstate!
How does Cobra compare to exchange plans (ACA, Obamacare, etc)?
We've written a full guide comparing Cobra to Texas Exchange plans.
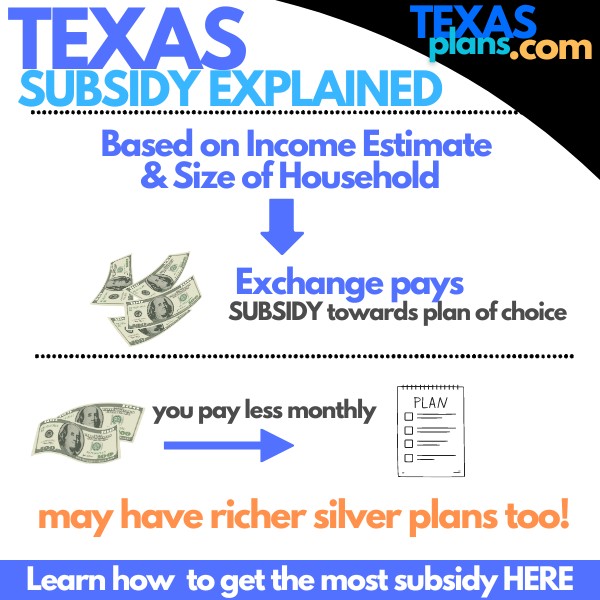
Many Texans opt for exchange plans if they qualify for subsidies, which can bring down the premium significantly. Check your subsidy eligibility here.
How does Cobra compare to short term health plans?
If Cobra is too expensive, short-term health plans can bridge the gap, especially if you're between jobs. Learn more about short term options here.
Short-term plans are usually much cheaper than Cobra, but they don't cover pre-existing conditions or offer as comprehensive coverage as exchange plans.
Check out our detailed guide on Cobra Coverage in Texas explained or Cobra versus Individual Famliy plans.